Frozen Shoulder
Frozen shoulder is a common condition in which the shoulder stiffens, reducing its mobility.
It commonly affects people aged between 40 and 60 years, and it is more likely in women than in men. It is estimated to affect about 3 percent of people.
It is also known as adhesive capsulitis.
The term “frozen shoulder” is often used incorrectly for arthritis, but these two conditions are unrelated.
Frozen shoulder refers specifically to the shoulder joint, while arthritis may refer to other or multiple joints.
The shoulder is made up of three bones: The shoulder blade, the collarbone, and the upper arm bone, or humerus.
The shoulder has a ball-and-socket joint. The round head of the upper arm bone fits into this socket.
Connective tissue, known as the shoulder capsule, surrounds this joint. Synovial fluid enables the joint to move without friction.
Frozen shoulder is thought to happen when scar tissue forms in the shoulder. This causes the shoulder joint’s capsule to thicken and tighten, leaving less room for movement. Movement may become stiff and painful.
The exact cause is not fully understood, and it cannot always be identified.
However, most people with frozen shoulder have experienced immobility as a result of a recent injury or fracture.
The condition is common in people with diabetes.
Risk factors
Common risk factors for frozen shoulder are:
- Age: Being over 40 years of age.
- Gender: 70 percent of people with frozen shoulder are women.
- Recent trauma: Surgery or and arm fracture can lead to immobility during recovery, and this may cause the shoulder capsule to stiffen.
- Diabetes: 10 to 20 percent of people with diabetes develop frozen shoulder, and symptoms may be more severe. The reasons are unclear
Other conditions that can increase the risk are:
- stroke
- hyperthyroidism, or overactive thyroid
- hypothyroidism, or underactive thyroid
Symptoms are usually classified in three stages, as they worsen gradually and then resolve within a 2- to 3-year period.
- Freezing, or painful stage: Pain increases gradually, making shoulder motion harder and harder. Pain tends to be worse at night. This stage can last from 6 weeks to 9 months.
- Frozen: Pain does not worsen, and it may decrease at this stage. The shoulder remains stiff. It can last from 4 to 6 months, and movement may be restricted.
- Thawing: Movement gets easier and may eventually return to normal. Pain may fade but occasionally recur. This takes between 6 months and 2 years.
Over 90 percent of people find that with simple exercises and pain control, symptoms improve. A frozen shoulder normally recovers, but it can take 3 years.
The aim is to alleviate pain and preserve mobility and flexibility in the shoulder. In time and with treatment, 9 out of 10 patients experience relief.
Painkillers: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are available to purchase over-the counter or online, and may reduce inflammation and alleviate mild pain.
Prescription painkillers, such as codeine, an opiate-based painkiller, may reduce pain.
Not all painkillers are suitable for every patient, so it is important to review options with the doctor.
PHYSIOTHERAPY
Transcutaneous electrical nerve stimulation (TENS): This works by numbing the nerve endings in the spinal cord that control pain. The TENS machine sends small to electrodes, or small electric pads, that are applied to the skin on the affected shoulder.
Shoulder manipulation: The shoulder joint is gently moved while the patient is under a general anesthetic.
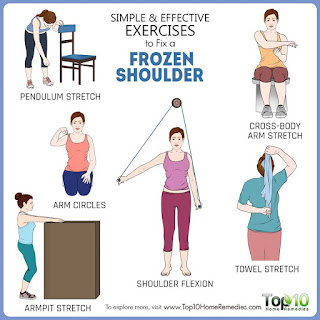
EXERCISES
PreventionFrozen shoulder can only be prevented if it is caused by an injury that makes shoulder movement difficult. Anyone who experiences such an injury should talk to a doctor about exercises for maintaining mobility and flexibility of the shoulder joint.
This can provide training in exercises to maintain as much mobility and flexibility as possible without straining the shoulder or causing too much pain.




👏🏻 great work shefali . .
ReplyDeleteVery nice shefhu be safe
Deletethanks siddhi
DeleteNice
ReplyDelete